DCIS Breast Cancer: Learn What You Need To Know
I’m a physician educator with the Breast Cancer School for Patients. In this article I’ll walk you through what DCIS (ductal carcinoma in situ) is, how it differs from invasive breast cancer, the treatment options you’ll encounter, the role of radiation and hormonal therapy, the link to BRCA genetic mutations, and how we decide when radiation might be safely omitted. My goal is to give you clear, practical information so you can talk with your surgeons and oncologists and make the best decisions for your care.
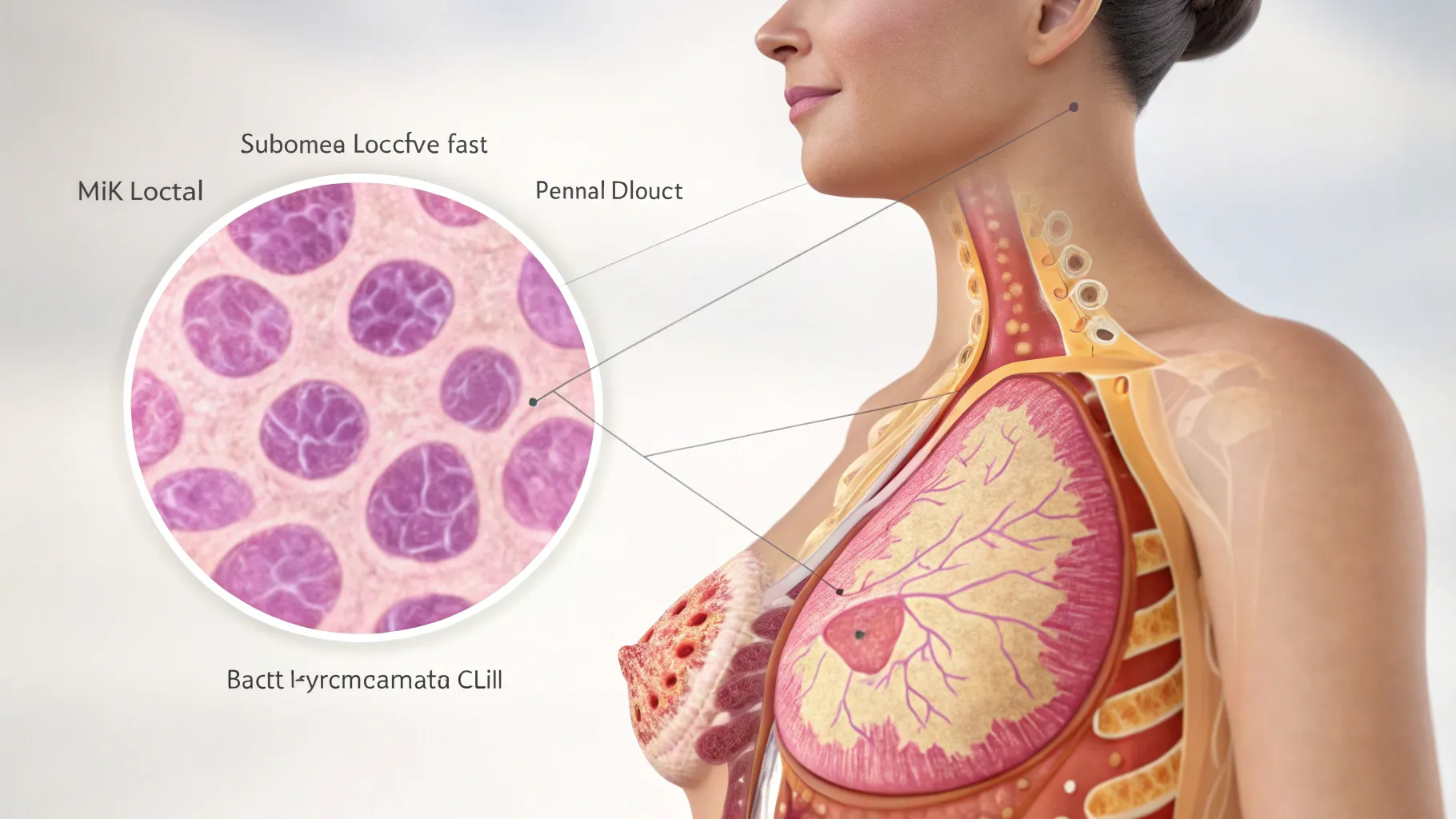
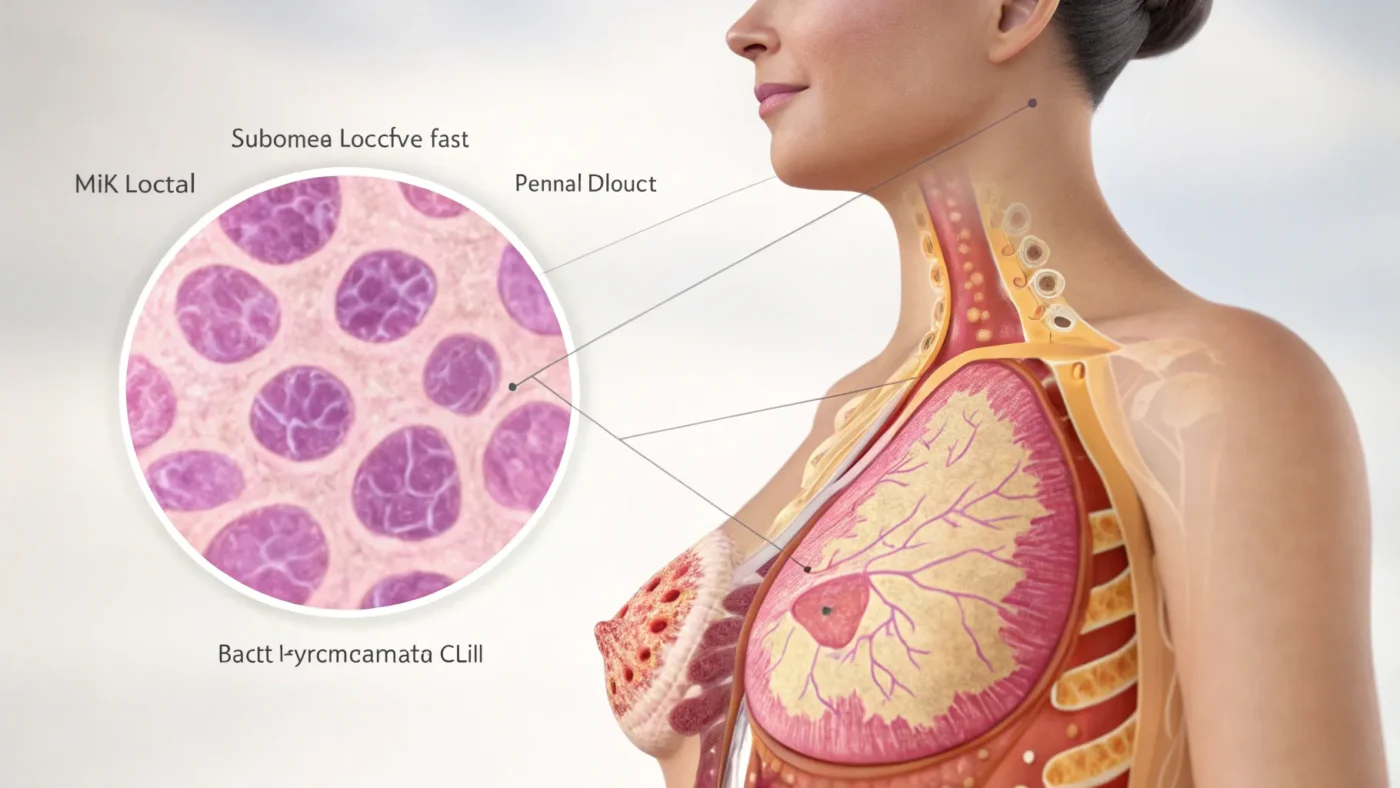
What is DCIS?
DCIS stands for ductal carcinoma in situ. It’s often called “stage 0” breast cancer. The simplest way to understand DCIS is that it’s an area of abnormal breast cells that have not yet gained the ability to invade outside the ducts and spread to other parts of the body. In other words, DCIS is a precancerous or very early cancerous condition rather than an invasive disease.
Key points about DCIS:
- DCIS is frequently detected on screening mammograms as calcifications (tiny white dots).
- It accounts for roughly 20% of breast cancer diagnoses.
- If left untreated, DCIS can evolve into invasive breast cancer over time.
How dangerous is DCIS?
When diagnosed and treated appropriately, the threat to your life from DCIS is very small. Large studies show the risk of dying from breast cancer 20 years after treatment with lumpectomy plus radiation is around 1%.
That said, having DCIS does change your future risk profile:
- Women who have had DCIS have a somewhat higher lifetime risk of developing a new breast cancer (in either breast) compared with women who have never had DCIS. For example, a woman in her 50s with no prior breast cancer might have a remaining lifetime risk of roughly 6–7%; after DCIS that risk can increase to around 10%.
- DCIS itself can recur locally after breast‑conserving surgery; half of local recurrences remain DCIS and half become invasive cancer.
Treatment options for DCIS
The mainstay of treatment for DCIS is surgery. The two broad surgical options are breast‑conserving surgery (lumpectomy) or mastectomy.
Lumpectomy (breast conserving surgery)
A lumpectomy removes the area of DCIS with a rim of normal breast tissue (a margin). Most women with appropriately small, localized DCIS are good candidates for lumpectomy. Because a tiny number of abnormal cells might remain even after an apparently complete excision, radiation therapy is commonly recommended after lumpectomy to reduce the chance of local recurrence.
Mastectomy
A mastectomy (removal of the whole breast) is generally recommended when DCIS is widespread or multifocal, or when the area is too large to remove with a reasonable cosmetic result. Some women also choose mastectomy for personal or risk‑reduction reasons. Radiation is usually not needed after mastectomy for DCIS.
Radiation therapy: when and why
Radiation following lumpectomy significantly lowers the chance of something coming back in the treated breast. Typical estimates (rounded):
- Lumpectomy plus a full course of radiation: about a 5–10% chance of a local recurrence over the next 5–10 years.
- Lumpectomy without radiation: roughly double the risk — about 10–25% chance of recurrence over the same period.
Radiation essentially halves the risk of local recurrence after breast-conserving surgery. Deciding whether to have radiation involves balancing this reduction in risk against the inconvenience and side effects of radiation and your personal preferences.
Hormonal (anti‑estrogen) therapy
Pathology testing on DCIS routinely checks for estrogen receptor (ER) and progesterone receptor (PR) status. If DCIS is ER‑positive, anti‑estrogen therapy (for example, tamoxifen or an aromatase inhibitor) may be offered.
Why consider hormonal therapy?
- It can reduce the risk of developing a new breast cancer (either DCIS or invasive) in the future by lowering the estrogen stimulation of breast tissue — a form of chemoprevention.
- It may also reduce the chance of a local recurrence in the treated breast.
These drugs have potential side effects, so a careful “risk vs. benefit” conversation with a medical oncologist is important.
Genetic testing and BRCA: what DCIS means for testing
DCIS can be associated with inherited mutations such as BRCA1 or BRCA2, although the majority of people with DCIS do not carry a BRCA mutation. If you carry a BRCA mutation, your lifetime breast cancer risk is substantially higher (commonly quoted in the 60–80% range for breast cancer), and your ovarian cancer risk is also increased (many estimates fall between 20–60%).
Important considerations:
- If you test positive for a BRCA mutation and you keep your breasts after DCIS, your lifetime risk of developing a new breast cancer can be quite high (often estimated around 50–60%).
- Genetic testing is commonly considered when DCIS occurs at a younger age (for example, under 50) or when there is a strong personal or family history of breast or ovarian cancer.
- A positive genetic result may change management: enhanced screening (adding MRI), consideration of bilateral mastectomy for risk reduction, or altered follow‑up strategies.
If you meet criteria for testing, discuss this with your surgeon or a genetic counselor as early as possible — it can influence surgical planning.
Can you avoid radiation after lumpectomy?
In most situations the answer is no — radiation remains an important part of breast‑conserving therapy for DCIS. However, there are selected circumstances where omission of radiation can be discussed:
- Older patients (for example, in their 60s, 70s or older) with very small, low‑grade DCIS and wide negative margins may derive limited absolute benefit from radiation, and omission may be reasonable.
- When an oncoplastic surgical approach allows removal of DCIS with a very wide margin (for example, a reduction‑type resection leaving large margins), the estimated recurrence risk without radiation may be acceptably low for some patients.
- Genomic assays that analyze the biology of the DCIS can provide additional information to help estimate local recurrence risk and guide the decision about radiation.
Any decision to omit radiation should be individualized and made collaboratively with your breast surgeon and radiation oncologist.
Genomic assays: looking deeper into the tumor
Newer tests (genomic assays) analyze the biology of DCIS cells and provide a risk score for local recurrence. One example is the Oncotype DX DCIS Score. When a patient is strongly motivated to avoid radiation and the traditional clinical factors look favorable, a genomic assay can add another piece of information to help weigh the decision.
Remember: genomic tests are only one part of the puzzle; they supplement — not replace — clinical judgment and specialist discussion.
Practical next steps and questions to ask your doctors
Being informed helps you make the best decisions. Ask your care team for a copy of your pathology report and discuss these topics openly. Here are some specific questions you can use:
- Is DCIS a cancer or a pre‑cancerous growth in my specific case?
- What exactly is the threat to my health from this DCIS?
- Are both surgery and radiation always needed for my DCIS?
- May I have a copy of my pathology reports?
- Do I qualify for genetic testing if I have DCIS?
- Will DCIS turn into an invasive cancer if it is not treated?
Additional practical tips:
- Discuss margins and the estimated risk of local recurrence with and without radiation.
- If pathology shows ER+ DCIS, ask about the pros and cons of anti‑estrogen therapy for prevention.
- If you are under 50 or have a strong family history, talk about early genetic testing and how results could affect surgery and screening.
- Consider getting opinions from both a breast surgeon and a radiation oncologist before finalizing a plan.
Final thoughts
DCIS is best thought of as early or precancerous disease that we catch before it becomes invasive. Treatment is effective and usually curative. While it can feel like aggressive treatment for a non‑invasive condition, the goal is prevention — to remove or neutralize abnormal cells before they can threaten your life.
Be informed, be proactive, and work with a multidisciplinary team (surgeon, radiation oncologist, medical oncologist/genetic counselor) to tailor the plan to your values and risk profile. If you want more structured education and a checklist of questions for your next visit, consider the resources available through the Breast Cancer School for Patients and register on our site to get a patient prep checklist and additional lessons.
You’re not alone — with the right information and team, most people with DCIS do very well.










Leave a Comment